Every month, Faculty of Computer Science Associate Professor Dr. Derek Reilly (PhD’09) gets together with older adults in the community for activities such as ping-pong, dancing, and miniature golf.
These get-togethers are not all fun and games, however. At least not for Dr. Reilly. He is one of several Dal researchers who are participating in ABLE Village, a multi-university study that is exploring how digital technology can support healthy aging. The ping-pong, dancing, and miniature golf—all of it is happening in the realm of virtual reality (VR). Dr. Reilly is using these get-togethers to look at how that technology changes, or even enhances, the way that older adults engage in socialization, creativity, and movement.
“We’re seeing older adults who want to sit down while they are playing a game or who have issues with using controllers due to arthritis,” Dr. Reilly explains. “Most of the gaming apps they are using haven’t been designed with accessibility and universality in mind.”
“We’re seeing older adults who want to sit down while they are playing a game or who have issues with using controllers due to arthritis. Most gaming apps they are using haven’t been designed with accessibility and universality in mind.”
This is where Dr. Reilly’s expertise in human-computer interaction comes into play. The observations and feedback he gathers at each get-together are informing new guidelines he is developing for creating more inclusive VR gaming apps. He plans to use these guidelines to design and launch his own proof-of-concept app through ABLE Village. This work could, quite literally, be a game changer.
“We have seen that these apps have the potential to reduce the barriers for participating in social and physical experiences among older adults, and that participation could have significant benefits for their physical, emotional, and mental health,” Dr. Reilly says.
“But there are a range of issues we will need to address, like eye strain and sensory conflict.” Dr. Reilly’s work represents a new era for the field of healthy aging. For years, it was dominated by companies promoting extracts, supplements, and other products making specious claims about turning back the clock.
Today, it is more scientifically rigorous and innovative, and Dalhousie University has played a lead role in that shift.
Leading the shift
Across the university, researchers are working to better understand the environmental and genetic factors that contribute to frailty both in older age and across our lifespans. They are exploring ways to make our communities more accessible and create smart homes that can detect daily patterns that signal cognitive or physical decline. They are also advocating for systemic changes in how health professionals view and deliver care to older adults.
These efforts reflect how complex and multifaceted the concept of healthy aging is. But they have two key aims: to keep older adults on a healthy trajectory so they can age in place in their homes and communities as long as possible; and to find ways to get people back on track when health issues result in hospitalization. This work is also helping Dal attract more partners, researchers, and students who are equally invested in exploring what healthy aging means and how best to achieve it.
A first-of-its-kind tool
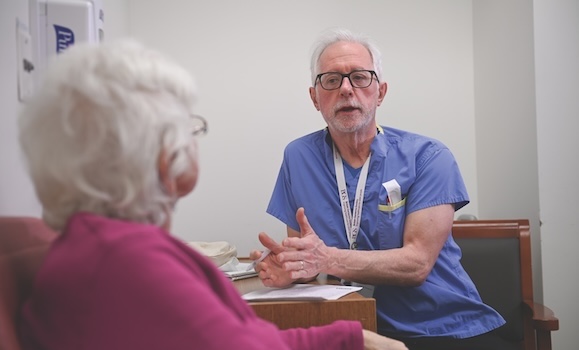
Dr. Kenneth Rockwood (PGM’91) is at the fore of Dalhousie’s efforts. The former Kathryn Allen Weldon Professor of Alzheimer Research is a world-renowned expert on geriatric medicine and frailty whose work is reshaping the delivery of acute care among older adults during hospitalizations. He co-developed the Clinical Frailty Scale, a first-of-its-kind tool for assessing the degree of frailty among older patients that has been adopted internationally. He has also conducted studies demonstrating the value of physical activity in preventing or reducing dementia and in preventing decline in health during hospitalization.
Dr. Rockwood’s work is driven as much by his concerns about the ageism and pessimism that he has witnessed in the treatment of older adults as it is by demographic trends that necessitate new approaches to care. In 2021, the first wave of baby boomers turned 75 and many more will reach that milestone in the years to come. That creates significant challenges for the world and for Atlantic Canada in particular. For one, that is the age at which most of the diseases of old age accelerate.
At the same time, more than 22 per cent of the region’s population is 65 or older—a percentage that not only surpasses that of any other region in the country, but is also going to grow. That will have ramifications for our health-care system in terms of demands and costs, and the impacts will ripple through society.
“We are not fully prepared for that,” Dr. Rockwood admits. “That’s on people like me, who were not persuasive enough with our arguments, our data, or our approach to show that we have to adapt. But it is also great to have a voice that says we need to change things and here’s how we do it.”
Related reading: Giant of geriatric medicine Dr. Rockwood named to Order of Canada
Dr. Rockwood is working toward system-wide change that would, in his words, effectively “geriatize” routine care. He wants to see more medical students become geriatricians and more doctors exposed to geriatric expertise in delivering care. That will require more encouragement and expansion of programs. For example, Dal is currently restricted to no more than three geriatric fellows every two years. By increasing these numbers, he believes it will be possible to address the fact that acute care is often a source of net harm for many older adults.
“In acute care, we often commit the great sin of treating the one thing we feel to be important when patients are presenting with four or five issues,” Dr. Rockwood explains. “But we’re trained to do that and we evaluate hospitals based on the most responsible diagnosis they can make when a patient shows up. What I want is for doctors to see opportunity—to be able to look at older patients and know immediately what to do for them or, failing that, to have on-site access to a skilled geriatrician who can help them.”
"What I want is for doctors to see opportunity—to be able to look at older patients and know immediately what to do for them or, failing that, to have on-site access to a skilled geriatrician who can help them.”
A lifespan approach
Dr. Olga Theou is taking a slightly different approach to looking at the issue of frailty. The Canada Research Chair in Physical Activity, Mobility, and Healthy Aging with the Faculty of Health’s School of Physiotherapy is interested in what happens across the entire lifespan that can contribute to or compromise someone’s ability to stay healthy.
“We see some people who age very successfully and others who develop significant health problems at a very young age,” says Dr. Theou, who co-developed the Pictorial Fit-Frail Scale with Dr. Rockwood, a tool that uses simple visual images to assess a person’s level of fitness-frailty. “We’re doing frailty studies among people as young as 20 to try and better understand the factors that lead to differences in health among our aging population. By understanding that, it is possible to individualize approaches based on each patient’s needs instead of approaching older adults like they all have the same needs.”
Through this lifespan approach, Dr. Theou is identifying interventions that can promote healthy aging. Her main interest is the benefit of physical activity. Through clinical and population-based studies in collaboration with Dr. Rockwood and other researchers, she has found that regular activity boosts health and reduces or defers frailty among older adults.
“When I say physical activity, I don’t just mean exercise, like when you go to the gym,” Dr. Theou explains. “I mean how much you move during the day, how much time you spend sitting down versus standing—so more like daily activities. These activities have one of the biggest overall impacts on our health. Many of the people that we see who are 100 years old and very healthy are more likely very active and doing lots of things during the day.”
Related reading: Government of Canada invests in first-of-its-kind research study on the health impacts of inactivity
Environmental impact
It is not just physical activity that contributes to healthy aging—it’s also the places we live. That’s what Dr. Liesl Gambold, an associate professor with the Department of Sociology and Social Anthropology, has found through her research. She’s been looking at retirement communities in Europe specifically designed for older 2SLGBTQIA+ populations and has noted their popularity and positive impact among members.
However, these populations remain underserved in Canada and Nova Scotia despite the presence of retirement communities that cater to a wide range of different demographics.
“We know that 2SLGBTQIA+ retirement communities are needed and desired because when homes were opened in Berlin and Stockholm, not only were all the available spaces filled, but there were also sizeable waitlists,” Dr. Gambold says. “What I found was that even if you have family support, people feel more vulnerable as they age. Being in a place where you can be out and live authentically helps to reduce that feeling of vulnerability in terms of emotional, psychological, or physical abuse.”
Dr. Gambold has also been looking at other ways that countries support healthy aging in the home and the community that could be readily and cost efficiently adopted here. For example, there are community facilities such as public parks and gardens and soccer fields in countries like Vietnam and Iceland that offer dedicated free time each week for older adults to engage in physical activity. There are Scandinavian countries that provide tablets to older populations so that regular health check-ins can be done. “It takes government support to make initiatives like these happen, but they have been shown to improve quality of life for older adults,” she says.
Read more in The Local Sweden: Sweden opens first retirement home for 2SLGBTQIA+
Incorporating AI
But what if your entire home could be equipped with technology that monitors and warns of declines in your health? That’s what Dr. Raza Abidi is working on. The Faculty of Computer Science professor and director of kNowledge Intensive Computing for Healthcare Ecosystems (NICHE) Research Group is developing an AI-driven platform to support ambient assisted living, a concept that involves equipping homes with smart sensors to capture data on an individual’s everyday activities such as when they wake up, when they take their medicine, and when they go for their daily walk.
“We have developed a set list of activities to capture, monitor, and assess using artificial intelligence that do not involve capturing audio or video,” Dr. Abidi says. “By establishing baseline patterns, we can then see if there are any long-term changes in the times or frequency of activities, interpret how or why they are happening, and provide necessary recommendations and proactive interventions that could help keep people in their homes. From a societal and family standpoint, this project has the potential to be transformative.”
Planning for accessibility
Equally transformative is the work being done by Dr. Mikiko Terashima (MSc'10, PhD'11), associate professor at the School of Planning and the associate dean of research and global relations with the Faculty of Architecture and Planning. She leads the Planning for Accessibility, Equity and Community Health (PEACH) research unit. Unique among planning schools, this team of dedicated faculty members, students, and community partners is training a new generation of planners to think about healthy aging in communities. It is also encouraging better planning practices by engaging individuals with lived experiences on the challenges they face in navigating the built environment in their communities.
“When it comes to accessible and inclusive environment, older adults and persons with disabilities are the experts. "
“When it comes to accessible and inclusive environment, older adults and persons with disabilities are the experts. We gather data on their perspectives and then we ask them for their suggestions on how to improve the design of their communities,” Dr. Terashima says. “For example, we are creating a 3D model based on these suggestions and show the research participants what our environment could look like if their suggestions were incorporated—what it would look like if we’ve got it right. Then, planners can learn from the visualized knowledge and make changes to enhance accessibility.”
According to Dr. Terashima, safety issues—and traffic safety issues in particular, such as unplowed sidewalks and traffic lights that change too fast—pose challenges to many older adults in navigating the built envnironment in the community. Other factors such as sidewalk widths and accessible parking spaces at places like supermarkets can also make daily activities and errands difficult for older adults, or persons with different types of disabilities, if they are not designed with their abilities and needs in mind.
“Once you start looking into these challenges, you realize they are all related, and that they have a profound impact not just on the ability to get into or use a space, but also navigating the whole journey from home,” Dr. Terashima says. “That’s why it is vital to more holistically assess built environment features to see where we can make improvements. It’s not just older adults and persons with disabilities who benefit; it’s everyone.”
Related reading: Planning students show community spirit with placemaking projects
The power of collaboration
Even as Dal researchers continue to make progress on issues related to healthy aging through their own projects, there is a strong interest in increased collaboration both across the university and with community partners to garner more insights and deliver more solutions. That interest is being fostered in part by Shannex, which operates several long-term care and residential facilities. It made a $2-million gift through Bringing Worlds Together to create the Shannex Chair in Artificial Intelligence and Healthy Aging.
The chair will work with the faculties of Health and Computer Science to develop predictive models to enhance the safety and well-being of older adults, as well as strategies for enhancing long-term care systems and health outcomes. The gift will also support the creation of the Shannex Research Lab in AI and Healthy Aging, which will promote interdisciplinary collaboration and research on health and frailty among older populations.
“Shannex is interested in the predictive potential of artificial intelligence to create solutions that will optimize care delivery and enhance resident experience in their facilities,” says Dr. Shaun Boe, professor and associate dean of research with the Faculty of Health. (Please note: Dr. Boe was recently appointed dean of Western’s Faculty of Health Sciences).
“At the same time, they are also interested in the preventative side of healthy aging so that people who come to their facilities can live there independently longer, enjoying a better quality of life. That means we are both helping them deal with the current aging crisis and preventing the situation from getting worse.”
The Shannex research lab will be co-located in the university’s Collaborative Health Education Building with an equally bold new initiative scheduled to open in fall 2025—the Dalhousie Healthy Aging and Frailty Hub. With infrastructure funded by the Canadian Foundation Dr. Raza Abidi and Dr. Olga Theou for Innovation and Research Nova Scotia, the hub will take an interdisciplinary approach to better understand the aging process, bringing together expertise in geriatric medicine, physiology, rehabilitation, neuroscience, cognitive science, and computer science.
“We are going to collect data about the body, people’s behaviour, frailty levels, cognition, and biomarkers, plug that into predictive models, and identify the factors that are changing the trajectory of healthy aging,” Dr. Boe says. “Based on that data, we can develop strategies to get people back on track and incorporate technology such as sensors to monitor adherence and progress, and how well the strategies are working. But the real goal is to scale the interventions we develop for the benefit of the community.”
Related reading: Shannex invests in healthy aging research at Dal with $2‑million gift
Visions for success
There is much more healthy aging research and education underway at Dalhousie, and even more is planned both in response to the current crisis and to prevent future ones from happening. There are also visions for what success will look like. For Dr. Rockwood, it means doing more for people in the community. That could include hospitals sending more acutely ill patients home, where they are likely to receive better care, or retirement communities that give as much priority to accessibility and public spaces for activity and socialization as they do private spaces.
“We need to look at our aging population as an opportunity,” Dr. Rockwood says. “When we meet their needs, we not only find new ways to tackle an international health crisis, but we also get more people talking about what else can be done to solve an issue that is not going away.”
Dr. Theou agrees, adding that, “We have medicine and technology that allow us to live much longer. The key is to ensure that doesn’t mean we live with reduced ability. That is why the research we are doing at Dalhousie is so important. It will lead to solutions so that most people can age healthy in their home and their community.”
“We have medicine and technology that allow us to live much longer. The key is to ensure that doesn’t mean we live with reduced ability. That is why the research we are doing at Dalhousie is so important. It will lead to solutions so that most people can age healthy in their home and their community.”
This story appeared in the DAL Magazine Fall 2024 issue. Flip through the rest of the issue using the links below.